Genes are the focus of a joint study at Bentley University and Gravity Diagnostics into how genetics affect a person’s likelihood of becoming addicted to opioids.
The National Institute of Health was looking for corporate academic partnerships to explore if a person’s genetic makeup can predict their risk of abuse.
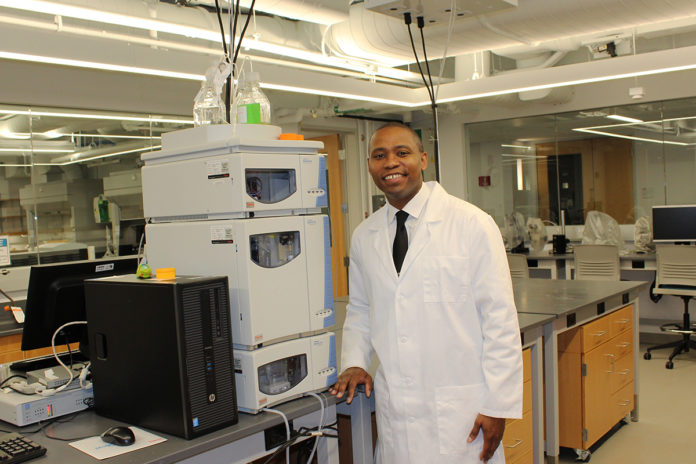
The research will explore individuals’ DNA to see how susceptible they may be to becoming addicted to opioid and whether those already addicted will respond to therapy, according to Christopher G. Skipwith, Assistant Professor of Biotechnology at the Department of Natural & Applied Sciences for Bentley University.
“One of the things that I have been doing for a while is looking at biomarkers that are related to disease and then establishing those biomarkers as valuable tests for diagnostic devices,” Skipwith said. Among the research, the scientists will look at genetic markers and the ability for someone to break down a specific drug, including prescription medications.
“It does have a lot of functions and a lot of things that can relate to how physicians treat various disorders based on how drugs can interact,” said Skipwith. That could have a great impact on decisions made by doctors when prescribing opioids, including how much to prescribe.
“What the project actually is looking at is susceptibility to opioid use and what we call OUD, opioid use disorder,” Skipwith said. “And what we do know is that there are many studies that have indicated that genetics can contribute up to 44%, or even higher in some cases, of variants that exists within opioid use disorder,” he said. “That addresses whether or not someone will actually become addicted to opioids if they are exposed chronically.”
How susceptible is someone on becoming dependent on opioids? What’s the best response to a patient following a course of treatment, including post-surgical treatment?
“It could relate to the ability of someone to actually respond to medication-assisted therapy or opioid replacement therapy,” said Skipwith. “Since there is such a highly correlated genetic background, what we figured is that we could use a lot of those factors and combine it into a risk assessment tool.”
This collaboration is about more than genetics since much of the information is already known.
“What we are doing is taking a lot of existing clinical results and then combining them into something that makes sense clinically,” said Skipwith.
The study could have an economic as well as a health impact, including financial savings for providers and insurance companies.
“How many lives does it save? How many trips to the emergency department does it save?” asked Skipwith. Only time will tell how the research will help.